Call Us Back
Kindly fill the above infomation and one of our executive will call you in 48 Hr.

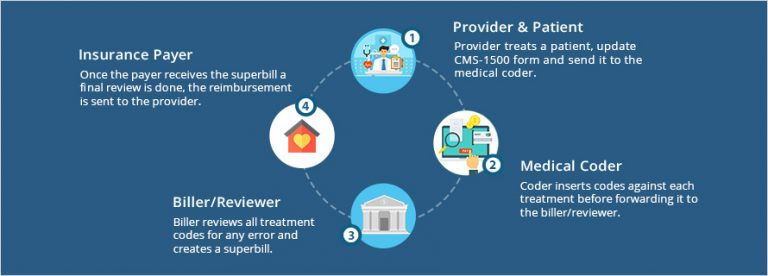
Medical Billing, in the United States, is used primarily for reimbursement purposes since the codes allow for efficient and accurate billing. We all know what an insurance claim is, ad Medical Billing is the process of submission and follow up on these insurance claims by insurance companies for the services provided by the healthcare provider.
The Medical Biller more so acts as a middleman between patients, healthcare providers and the insurance companies. Their job, is on similar lines in context to the Medical Coder. The Medical Biller translates the codes given by the Medical Coder into a financial report, they make sure that the Healthcare Provider has been reimbursed appropriately for the services they've provided. Do not be fooled by the simplicity of the term "Medical Billing", it may seem that all the Medical Billers task is to make a bill (Commonly known as a 'Claim') for the insurance company by the help of the information provided by the Medical Coder, the reality of the process is not as simple.
Talking about the word 'Traditional' you must have got an idea that it requires ALOT of manual documentation and paper work, the average time for a traditional coding and billing process stretched on to about 5-7 weeks whereas in the modern automated system the process is reduced to as low as 2 weeks.
Following is a Claim-to-Payment Chase while using a traditional Paper-Based System.
Now the point where AI fits into the story is to enhance the efficiency and efficacy of the billing and coding process. Computer Assisted Coding (CAC) is a technology that works on the concept of Machine Learning (ML) which is a branch of Artificial Intelligence (AI) and Natural Language Processing (NLP), they provide automated assistance to the rigorous task of identifying and extracting data from the given documents and inserting it into the system.
- AI can automate a web-based system that’s used to analyse a physician’s documentation for the treatment and recognise the relevant medical codes from its pre-defined medical coding list. The benefits of medical coding using AI is that it can automate the detection of predefined medical billings codes used by insurance companies.
- Today, the ongoing challenge is the coding accuracy. To improve the efficiency and efficacy of the billing and coding process, many healthcare companies are finding ways to simplify manual coding labor with AI applications.
- The emerging technology in AI is based on Computer Assisted Coding (CAC) which works on Machine Learning and Natural Language Processing (NLP). The CAC automatically identify and extract data from documents and insert into the system.
- The need of the hour is an automated web-based system that analyzes physician documentation for the text/treatment and automatically recognizes relevant medical codes.
- Beyond processing codes and high volumes of data, AI can significantly reduce the standard work hours and human error.
- Applying AI in Medical Billing to reduce overall costs and increase efficiency across the industry
- As one might guess, improved accuracy is one of the major draws to bringing AI into the medical billing and coding industry. However, accuracy doesn’t just stop at analyzing texts and records to determine which procedures require billing.
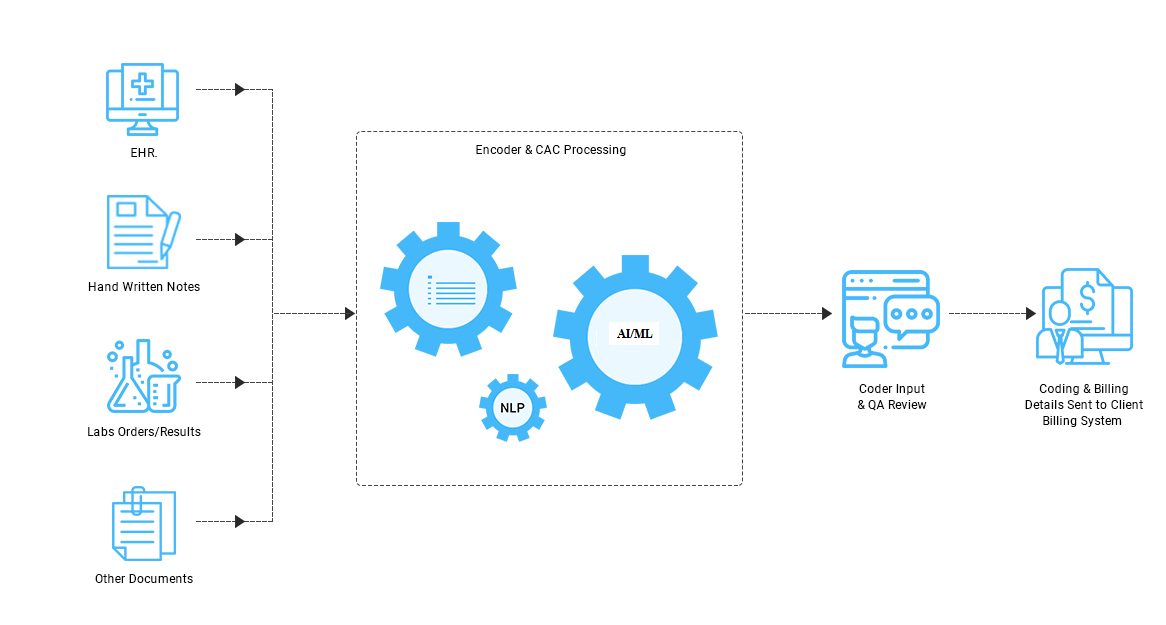
The above image demonstrates the creation and usage of AI in the form of softwares and NLP (Natural Language Processing), here, used in the process to generate a medical report.
We offer the most advanced technology that is poised to streamline the medical billing and coding industry, the Computer Assisted Coding (CAC) technology for AI in billing. This technology enables machine Learning and natural language processing to extract relevant data and insert it into the specific fields of billing in an automated fashion. The intelligent analysis of physical documents that allows recognition of relevant code and their application is the distinct advantage of this technology.
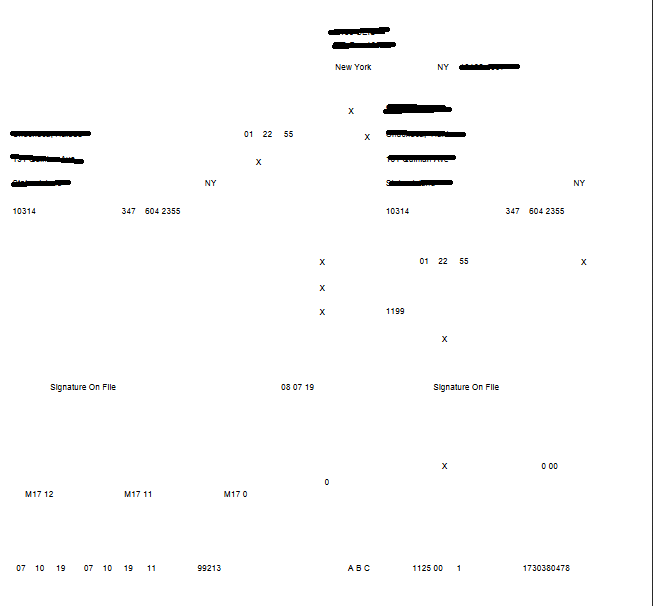
Sample claim form
Medical billers and coders can heave a sigh of relief to the constant hassle of denied or rejected claims through the adoption of our data anomaly detection feature for AI in billing. This superior solution detects anomalies based on historically fed information of denied and rejected claims and brings them to the attention of coders and billers through an alert system. The number of denied and rejected codes is substantially reduced through this preventive method.
Our AI billing solutions are designed to target the entire workflow of the medical billing process for holistic optimization and thereby increase overall revenue. Ranging from identifying and targeting vulnerable areas in the billing system, to a considerable reduction in tedious tasks through automated features, the AI billing technology optimizes the complete lifecycle of medical billing and coding.
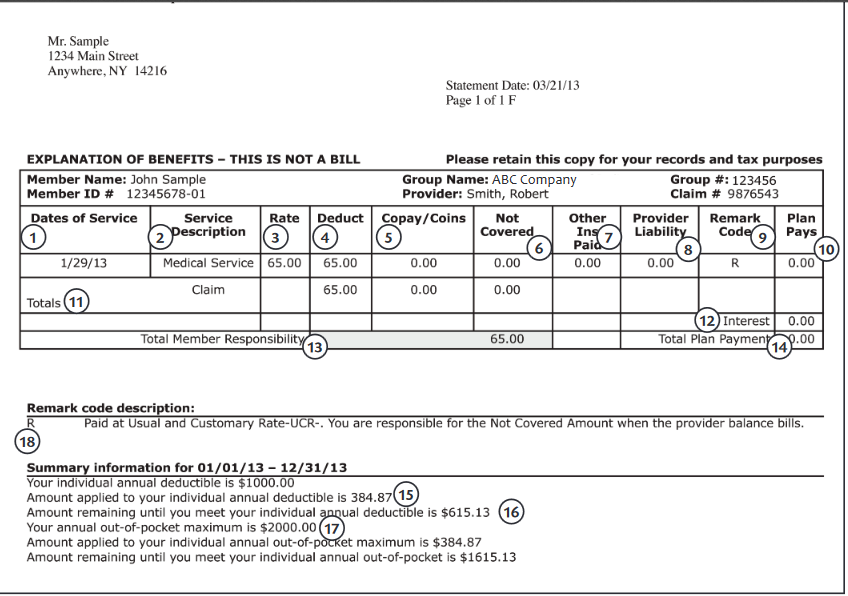
Sample PDF screen of medical bill
AI-powered healthcare revenue cycle is, overall, a future of all medical billing as it moves towards the digitalised practice. The automation and efficiency it offers are a winning combination that many more healttech providers should be able to access.
One of the issues that leads to declined insurance claims is the inaccuracy of billing codes. Insurance companies are cautious about improper billing procedures, and one error can cause a claim to receive reduced, or no payout. Higher accuracy, thanks to AI assistance, would help reduce this problem.
As one might guess, improved accuracy is one of the major draws to bringing AI into the medical billing and coding industry. However, accuracy doesn’t just stop at analyzing texts and records to determine which procedures require billing.
The list of medical codes doesn’t have large-scale changes often, but there are still updates that better reflect the needs of health care providers. In 2019 alone, there will be 392 new codes, 216 deleted ones, and eight revised titles. Complete revisions of the coding standards can also occur, which can involve substantial adjustments to new and existing codes.
While the medical industry can adjust to these changes as it has before, it does take time. And in that time – especially right after an update – the learning curve can lead to more errors as coders become used to the new codes and procedures.
AI systems could help better facilitate these adjustments in many ways. One example could be in suggesting new codes or preventing entering codes that no longer exist, as well as reminding users of any changes a code has gone through. Guided prompts would speed up the process of coders adapting to whatever changes may arise in the future.
One of the other complications the medical billing and coding industry faces, besides accuracy issues, is in processing time. Currently, it takes a long time for a procedure to be billed, and then additional time for insurance companies to accept that bill and distribute payment. These backed-up payments are a problem for patients, providers, and insurance companies alike.
Improved processing times begin with the coders. All the processes we’ve mentioned above, especially accurate text processing, can save coders time in compiling procedure and billing information. The time saved with this increase in coder efficiency can then speed up the rest of the process, benefitting everyone.
When less time and resources go into compiling bills, medical professionals can focus more of their efforts into maintaining accuracy in more complicated coding scenarios and providing higher-quality patient care. These outcomes can potentially improve the cost of health care services and health insurance.